History of Antibiotics
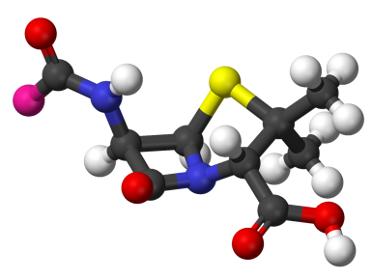
Table of Contents
- Importance of the Discovery of Antibiotics
- History of Antibiotics before Fleming's Discovery of Penicillin
- Discovery of Penicillin by Alexander Fleming
- Development of the Technique for Mass Production of Penicillin by Howard Florey and Ernst Boris Chain
- Discovery of Streptomycin by Selman Waksman
- History of Antibiotics After the Mid-1940s
- Antibiotic Resistance and A Glance into the Future of Antibiotics
Quick Facts
Antibiotics in a form of selected molds and plant extracts were used already in ancient times but their mode of action was not understood until the 20th century.
Alexander Fleming discovered the first antibiotic - penicillin in 1928 by accident.
The Scottish bacteriologist noticed that a blue-green mold on a contaminated culture plate killed the Staphylococcus aureus bacteria.
Fleming continued to work with the mold he identified as Penicillinum notatum and came to conclusion that the substance it produces - penicillin has the ability to kill the disease-causing bacteria without being toxic to healthy cells.
In 1941, Howard Florey and Ernst Boris Chain succeeded where Fleming had failed - producing enough penicillin for clinical trials.
By 1945, the pharmaceutical companies started mass production of penicillin which, however, could not cure diseases caused by Gram-negative bacteria.
In 1944, Selman Waksman announced the discovery of streptomycin, an antibiotic that works against Gram-negative and the tuberculosis bacteria.
In 1945, Bejamin Duggar discovered aureomycin, the first from the class of tetracyclines that work against both Gram-positive and negative bacteria.
Discoveries of new antibiotics continued until the 1970s. Afterwards, the scientists mostly made only improvements within already discovered classes of antibiotics.
Antibiotics saved millions of lives worldwide but they are not as effective as they used to be due to antibiotic resistance caused by improper use and misuse of antibiotics in the previous century.
Importance of the Discovery of Antibiotics
The discovery of antibiotics, a group of medications which are used to fight disease-causing bacteria is considered one of the most important milestones in history of medicine. A number of previously incurable diseases were virtually eradicated and millions of lives have been saved after antibiotics became available to the general public in the mid-1940s. However, careless use and misuse of the “wonder drugs“ in the last 50 years have started to cause problems with antibiotic resistance and emergence of the so-called superbugs or super bacteria which are resistant to all available antibiotics.
History of Antibiotics before Fleming’s Discovery of Penicillin
History of antibiotics officially begins in the late 1920s when the Scottish bacteriologist Alexander Fleming (1881-1955) identified penicillin as an antibacterial agent, however, the use of antibiotics dates back to ancient times. The Chinese are known to use molds to fight infections as early as 2500 years ago, while medicinal folklore in Europe treated infections with plant materials and extracts some of which were later shown to have antibiotic properties. Chinese traditional medicine as well as European medicinal folklore achieved some success in treatment of infections with the selected molds and plant extracts but it was not until the 19th century when the scientists identified bacteria as disease-causing agents and started considering using microorganisms for curing infectious diseases. Among the first to discover the potentials of materials derived from naturally occurring microorganisms for medicinal purposes was the French chemist and microbiologist Louis Pasteur (1822-1895). He is best known for developing pasteurization but in 1877, he also discovered that saprophytic bacteria (bacteria that feed on dead or decaying material) can inhibit the growth of the disease-causing anthrax bacteria.
Discovery of Penicillin by Alexander Fleming
The breakthrough in history of antibiotics occurred in 1928 when Alexander Fleming accidentally discovered that the disease-causing Staphylococcus aureus bacteria were killed by a blue-green mold growing on an uncovered plate when returning to his lab after a month long vacation. He examined the mold and named it Penicillinum notatum that gave the name to the first antibiotic. Fleming started to experiment with the mold and injected the substance it produced - penicillin (or “mold juice“ as he called it) to mice. He discovered that penicillin kills the harmful bacteria without causing toxicity, however, he was not able to purify the substance nor produce it in large enough quantities to prove its value for medicinal applications. Fleming published his discovery in the Journal of Experimental Pathology in 1929 but his findings attracted little attention.
Development of the Technique for Mass Production of Penicillin by Howard Florey and Ernst Boris Chain
Not long after Fleming gave up trying to turn penicillin into drug, his article in the Journal of Experimental Pathology was noticed by Australian pathologist Howard Florey (1898-1968) and German-born British biochemist Ernst Boris Chain (1906-1979). In the late 1930s, the two scientists gathered a research team and succeeded where Fleming had failed - producing enough penicillin for clinical trials which began in 1941. The very same year, the scientists announced that penicillin could be used in humans to combat diseases but they had to travel to the United States to develop an effective technique for mass production of penicillin due to Britain’s involvement in World War II. In 1942, penicillin was distributed to the British soldiers and by 1945, enough antibiotic was produced to meet the demands of the general public. The success of penicillin was enormous and Alexander Fleming, Howard Florey and Ernst Boris Chain were awarded the Nobel Prize for Medicine in 1945.
Discovery of Streptomycin by Selman Waksman
Penicillin that came to be called the “wonder drug“ soon became the primary treatment for a number of diseases including bacterial pneumonia, gonorrhea, syphilis, scarlet fever, etc. but it could not cure all bacterial diseases. Penicillin works only against Gram-positive bacteria (those that retain blue or violet color in Gram stain test). It is ineffective against Gram-negative bacteria (those that do not retain blue or violet color in Gram stain test) as well as against mycobacteria that cause tuberculosis and are neither Gram positive nor negative. However, the discovery of antibiotic that works against Gram-negative and the tuberculosis bacteria followed soon. In 1944, Russian-born American microbiologist Selman Waksman announced that he had discovered streptomycin and claimed that it can cure tuberculosis. Clinical trials confirmed his claims and he was awarded the Nobel Prize in 1952. Waksman was also the first to use the name antibiotic (from Greek anti meaning against and biosis meaning life, literally meaning against life) for a substance that kills bacteria without being toxic to healthy cells.
History of Antibiotics After the Mid-1940s
Since the mid-1940s, a number of new classes of antibiotics were developed. In 1945, Bejamin Duggar discovered aureomycin, the first from the class of tetracyclines that work against both Gram-positive and negative bacteria (known as broad-spectrum antibiotics). Four years later, J. M. McGuire isolated erythromycin (usually used for patients who are allergic to penicillin) for the American pharmaceutical company Eli Lilly, while the Italian scientist Giuseppe Brotzu isolated cephalosporin one year earlier. Discoveries of new antibiotics continued until the 1970s. Afterwards, the scientists mostly made only improvements within already discovered classes of antibiotics.
Antibiotic Resistance and A Glance into the Future of Antibiotics
Mass use of antibiotics dramatically reduced complications and fatalities caused by bacterial infections but it also enabled the bacteria to catch up with the drugs. As a result, antibiotics are not as effective as they used to be and people started to die from infections that were easily treated just a decade ago. The scientific community therefore called for more responsible use of antibiotics (prescribing antibiotics only when really necessary and completing the entire course of antibiotics when prescribed for instance) to prevent the disease-causing bacteria from developing antibiotic resistance. However, bacteria will continue to evolve resistance as long as they will be exposed to antibiotics which is why new research and development of completely new antibiotics will be probably necessary in the future to avoid an antibiotic resistance crisis.